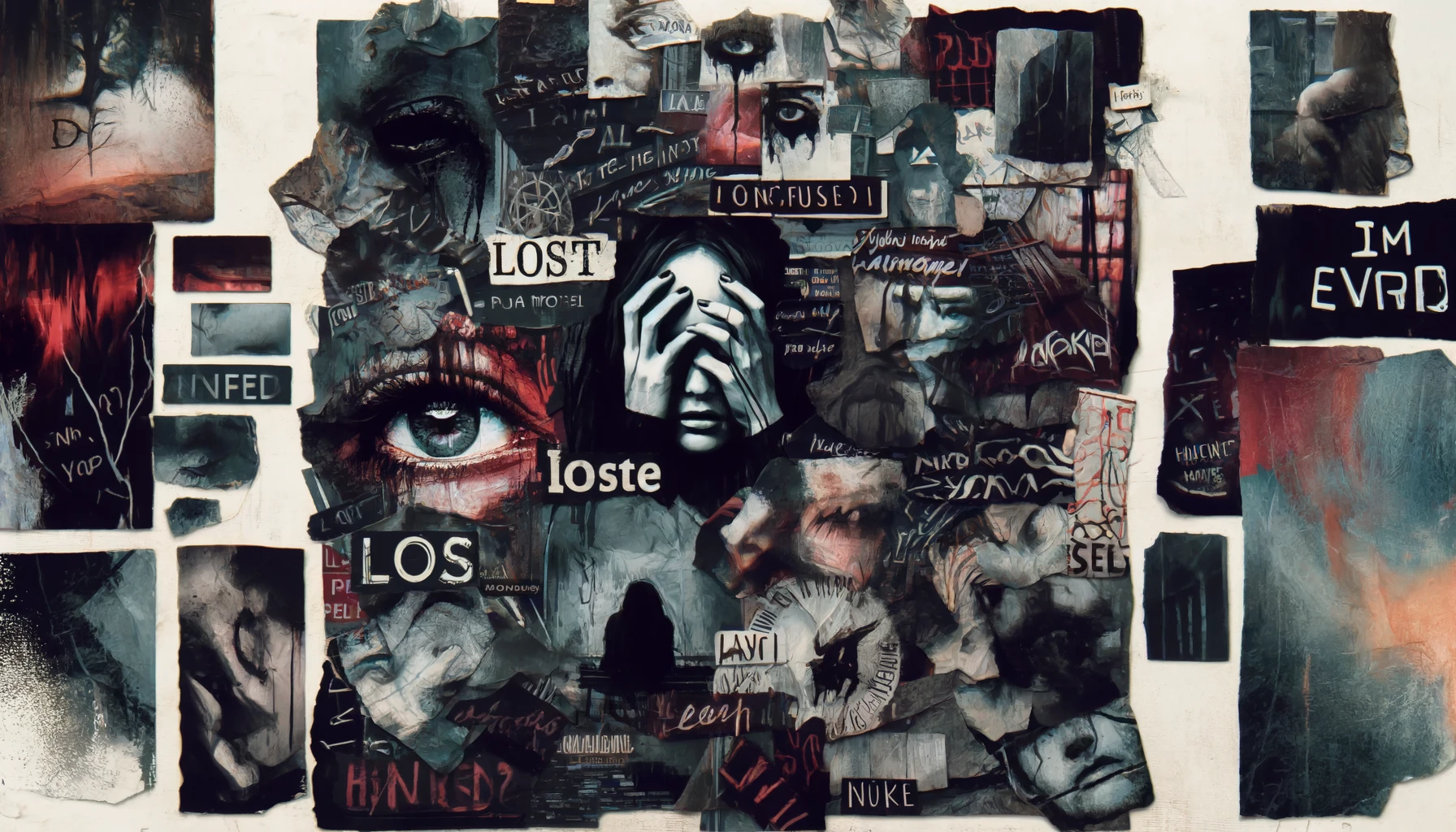
Borderline Personality Disorder (BPD) is a complex mental health condition characterized by unstable moods, behaviors, and relationships. It is often misunderstood and stigmatized, but with proper treatment and understanding, individuals with BPD can lead fulfilling lives.
What is Borderline Personality Disorder?
Borderline Personality Disorder is a mental health disorder marked by a pattern of ongoing instability in moods, behavior, self-image, and functioning. These experiences often result in impulsive actions and unstable relationships. The disorder typically begins by early adulthood.
Symptoms of BPD
The symptoms of BPD can vary but generally include the following:
- Emotional Instability: Intense and variable emotions that can change rapidly.
- Distorted Self-Image: An unstable self-image or sense of self, often fluctuating between extremes.
- Fear of Abandonment: Extreme efforts to avoid real or imagined abandonment.
- Impulsive Behaviors: Impulsive actions that may include spending sprees, unsafe sex, substance abuse, reckless driving, and binge eating.
- Unstable Relationships: Intense and unstable relationships with others, often swinging between idealization and devaluation.
- Chronic Feelings of Emptiness: A pervasive sense of emptiness or boredom.
- Inappropriate Anger: Intense anger or problems controlling anger.
- Paranoid Thoughts: Periods of stress-related paranoia or severe dissociation.
Causes of Borderline Personality Disorder
The exact cause of BPD is not known, but it is believed to result from a combination of genetic, environmental, and social factors.
- Genetic Factors: Studies suggest that people who have a close family member with BPD may be at a higher risk of developing the disorder. This indicates that genetics play a role in the development of BPD.
- Environmental Factors: Environmental factors, particularly those involving childhood trauma, are believed to be significant contributors. Experiences such as physical or sexual abuse, neglect, or separation from parents during childhood can increase the risk of developing BPD.
- Social Factors: Social factors, including how individuals interact with their family, friends, and other people, can also influence the development of BPD. Early attachment issues and instability in relationships can contribute to the disorder.
Diagnosis of BPD
Diagnosing BPD involves a comprehensive evaluation by a mental health professional. The process typically includes:
- Clinical Interview: Discussing symptoms, personal history, and family history with a mental health professional.
- Psychological Evaluation: Using standardized assessment tools to evaluate the presence and severity of symptoms.
- Medical Examination: Ruling out other medical conditions that might be causing symptoms.
Treatment Options
While BPD can be challenging to treat, several effective options are available that can help individuals manage their symptoms and improve their quality of life.
Psychotherapy
Psychotherapy, also known as talk therapy, is the primary treatment for BPD. Different types of psychotherapy have been found effective, including:
- Dialectical Behavior Therapy (DBT): Specifically designed for BPD, DBT focuses on teaching skills to manage emotions, improve relationships, and reduce self-destructive behaviors.
- Cognitive Behavioral Therapy (CBT): Helps individuals identify and change distorted thinking patterns and behaviors.
- Mentalization-Based Therapy (MBT): Focuses on helping individuals understand the thoughts and feelings of themselves and others.
Medication
While there is no medication specifically approved for BPD, medications can help manage specific symptoms such as depression, anxiety, or mood swings. These may include:
- Antidepressants: To treat symptoms of depression and anxiety.
- Mood Stabilizers: To reduce mood swings and impulsivity.
- Antipsychotic Medications: To treat symptoms of anger and paranoia.
Hospitalization
In severe cases, hospitalization may be necessary to ensure the safety of the individual and to provide intensive treatment in a safe environment.
Living with BPD
Living with BPD can be challenging, but with the right support and treatment, individuals can manage their symptoms and lead fulfilling lives. Here are some strategies that can help:
- Build a Support Network: Connect with family, friends, and support groups who understand and support your journey.
- Practice Self-Care: Engage in activities that promote physical and mental well-being, such as exercise, healthy eating, and mindfulness practices.
- Develop Coping Skills: Learn and practice coping skills to manage stress, emotions, and relationships effectively.
- Stay Committed to Treatment: Consistent engagement with therapy and treatment plans is crucial for managing BPD.

Borderline Personality Disorder is a complex and challenging condition, but with the right treatment and support, individuals can manage their symptoms and achieve a better quality of life. Understanding the disorder, seeking professional help, and building a strong support network are essential steps in the journey towards recovery.